 Care Management
Care Management
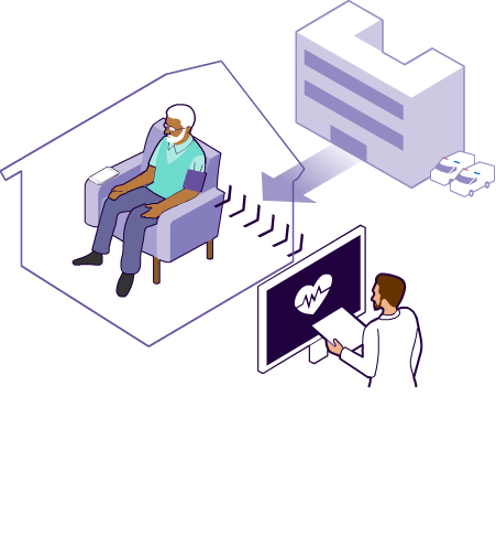
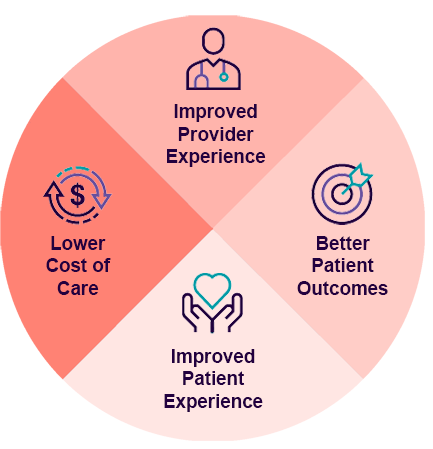
Innovista’s strength lies in care management—identifying high-risk patients who need extensive care and providing support along the care continuum. These efforts help strengthen provider-patient relationships while removing burden on office staff, which minimizes burnout and allows physicians to focus on the most important goal: keeping patients healthy. Care managers:
- Encourage use of and improve access to primary care services
- Prevent inappropriate emergency department use and readmissions
- Prevent or delay progression of chronic disease
- Remove barriers related to social determinants of health
- Coordinate care to increase quality measure scores and close care gaps
52%
More shared savings for providers who engage and refer to our care management team
We bring together a multidisciplinary team of nurses, social workers, care coordinators, community health workers, and community-based organizations to mitigate costs and improve patient outcomes through:
- Case management (complex, behavioral, and disease specific)
- Medication adherence support
- Annual wellness visits, nutrition coaching, smoking cessation, behavioral counseling, and obesity treatment/prevention
- Transitional care and emergency care follow-up
- Care delivered according to National Committee for Quality Assurance (NCQA) standards
- Centers for Medicare & Medicaid Services (CMS)-related compliance and community outreach initiatives
 Provider Enablement
Provider Enablement
Without understanding the unique characteristics of every provider network, it’s impossible to design a program to help them succeed in value-based care. Plus, it requires the right tools and support so providers can meet the many expectations of this healthcare model.
Innovista’s provider enablement team gives practices tools and technologies to help them succeed, scaled to meet their unique needs and ensure they don’t take on excess burden:
- Trainings, reporting, compliance, and site visits
- Innovative processes, reporting, and communication integration
- Strategic planning to drive enrollments
- Problem solving to ensure sustained provider satisfaction
 Quality Performance & Improvement
Quality Performance & Improvement
Improving care quality and achieving operational excellence is the foundation of value-based care. However, it can feel like an ever-moving target.
Developing a solid structured program that allows for fluidity of unexpected shifts in the paradigm of medicine is the key to success. Innovista provides a comprehensive quality performance platform and improvement solutions that help providers navigate through the complexities of value-based care:
- Chart audits to identify care gaps, recommend screenings and immunizations, discuss medication adherence, and leverage annual wellness visits
- EMR templates and standardized documentation to close gaps
- Transparent reporting that provides actionable recommendations
- Report management for multiple payer portals
- Validated supplemental data submissions
- Provider education and engagement to implement evidence-based workflows
- Trainings on CPT codes to ensure accuracy for closing quality gaps
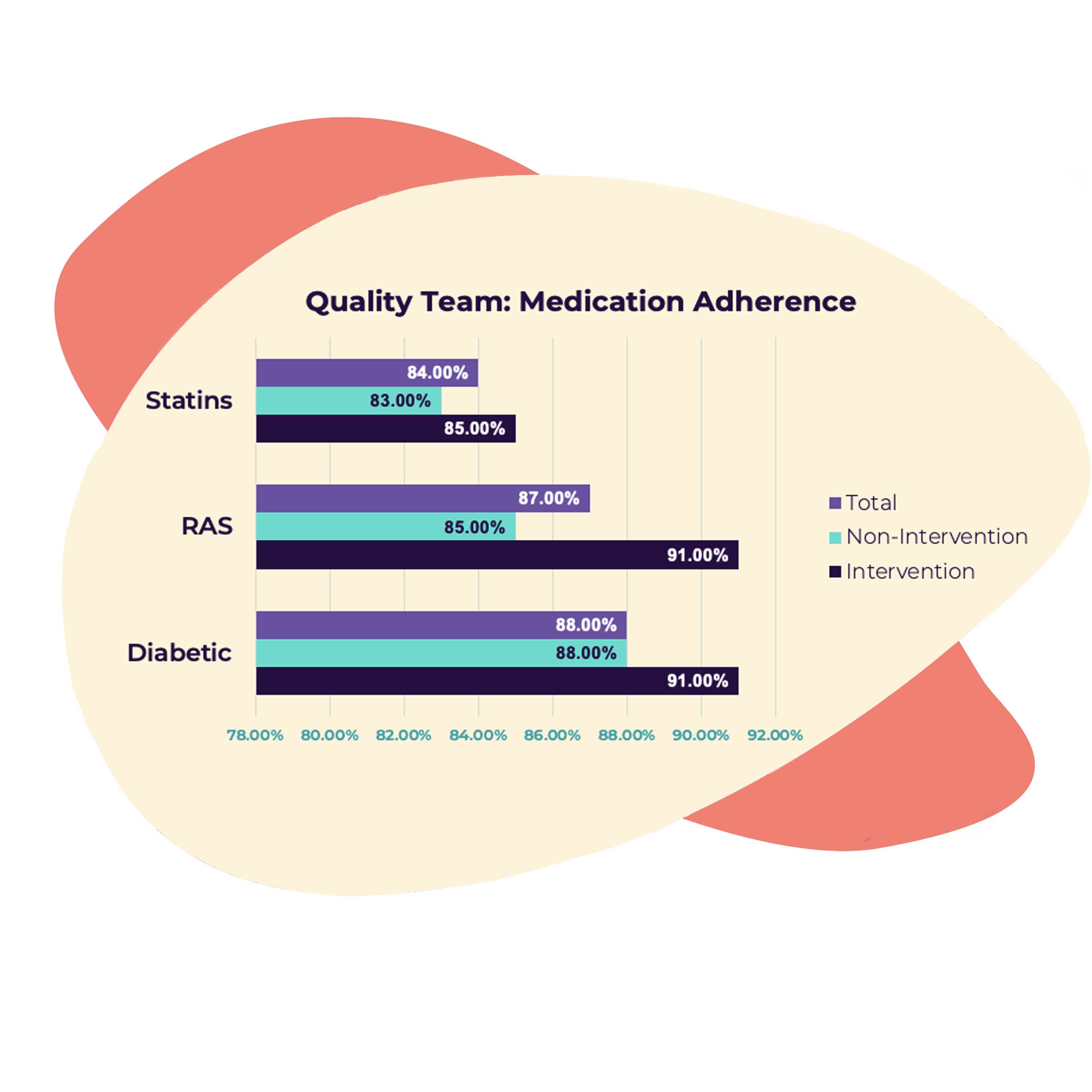
Quality performance success frequently results in higher distribution of shared savings and incentive payments.
 Risk Adjustment
Risk Adjustment
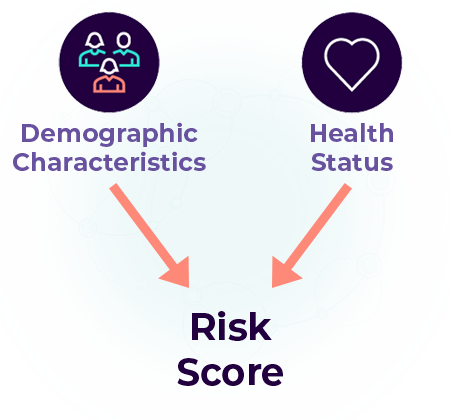
Innovista positions providers for financial success by:
- Focusing on coding accuracy and ensuring documentation meets compliance standards
- Educating providers and staff on coding and documentation requirements
- Supporting Medicare risk adjustment education and workflows
- Conducting risk adjustment audits to identify areas where risk scores can increase
- Creating Hierarchical Condition Category specific newsletters and trainings
- Measuring physician engagement and knowledge
Risk adjustment accounts for the differences in expected costs vs. actual costs of a patient population so that providers and payers can both be properly compensated. Successfully capturing and adjusting risk also enables providers to have a complete picture of each patient’s acuity, which helps care managers make informed recommendations for managing high-risk patients and delivering targeted care.
Innovista’s risk adjustment team positions providers for financial success in risk-sharing arrangements by:
 Performance Insights & Analytics
Performance Insights & Analytics
Innovista provides performance insights and analytics using business and critical data to offer meaningful insights, set benchmarks, and help providers take action.

- PCP engagement to gain actionable insights into patient and provider data, leading to improved outcomes, cost savings, and higher efficiencies
- Provider profiling to improve overall population health, healthcare operation efficiency, and quality
- Provider network development to create more efficient delivery systems and give feedback to PCPs
- Improvement in quality of care by identifying patterns and improved treatments
- Medical management services to reduce inefficiencies and identify cost-effective ways to deliver care
- Action plan development and implementation to improve business and patient outcomes
 ACO Enablement & Network Development
ACO Enablement & Network Development
Joining an accountable care organization (ACO) can strengthen primary care practices and help foster success in value-based care.
Reduced costs and better savings: ACOs reduced Medicare spending by nearly $2 billion in 2020.
Strategic partnerships: ACOs encourage independent physicians to collaborate with other providers to share resources and decision making.
Greater patient reach: Electronic physician network management systems make it easy for primary care providers to quickly search for specialists who meet quality-of-care standards when making referrals.
Patient retention and loyalty: ACOs foster better patient-provider communication.
Access to technology: ACO members have access to operational and administrative technologies that make it easier to safely transmit patient information between providers.
Our Clients








