Medicaid is an important part of the medical landscape, providing coverage for 85 million underserved people in America. In Texas, a key state of operation for Innovista Health, 5.3 million residents receive Medicaid benefits.
Social Determinants of Health’s Effects on Medicaid Population
While Medicaid is a lifesaver for millions of beneficiaries, there are specific challenges that often need to be addressed in this patient population, particularly relating to social determinants of health (SDOH). SDOH are underlying non-health factors that affect someone’s overall health and wellbeing:
- Lack of educational/employment opportunities
- Low access to nutritious food
- Poor literacy
- Environmental pollution
- Unsafe housing and neighborhoods
- Lack of transportation
Community Health Workers: Key Players in Addressing SDOH
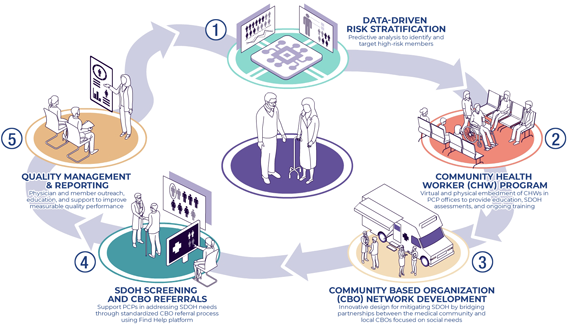
Community health workers (CHWs) are nonclinical healthcare professionals who support patients’ physical, mental, and social needs by connecting them to community resources and services. Since CHWs are very familiar with the communities they serve, they play a pivotal role in assessing patients for SDOH and addressing them in a sensitive, understanding manner.
Some of the biggest positive outcomes include higher rates of preventive screenings, better access to healthcare services, and increased adherence to medication and health recommendations.
Innovista has an experienced team of CHWs that work directly with patients and providers to help address SDOH and other areas of concern to improve patient health and outcomes.
Benefits of CHW Interventions
-

Reduced hospitalizations
-

Improved chronic disease control
-

Increased quality of care
North Texas ED Overutilization Success
Innovista’s partnership with a leading Medicaid insurer in the North Texas area afforded us the opportunity to work with and improve the lives of nearly 40,000 Medicaid beneficiaries, starting in 2019.
One of the biggest challenges to address was ED overutilization, which was nearly 50% higher than Medicaid’s national goal. Nearly 90% of patients who went to the ED were not admitted, which meant they didn’t need to be there.
CHWs were deployed to meet with these ED utilizers. They addressed SDOH in a sensitive, nonjudgmental manner, connected them with community resources, helped set up primary care visits, and educated them on alternatives to the ED.
Within nine months, ED usage dropped by 40%. The use of mobile urgent care service Dispatch Health alone saved $1.2 million in unnecessary ED visits. Outreach to one patient in particular lowered her ED visits from 69 in 2021 (total cost $34,305) to two unavoidable encounters in 2022 (total cost $711).
Physician & Payer Needs in a VBC Platform
Value-Based Care Platform
-

Provider Engagement & Management

Economic Model
-

Integrated Clinical Model

Financial Risk Management
-

Patient-Centered Product Offering

Data Platform
-

Analytics-Driven Insights
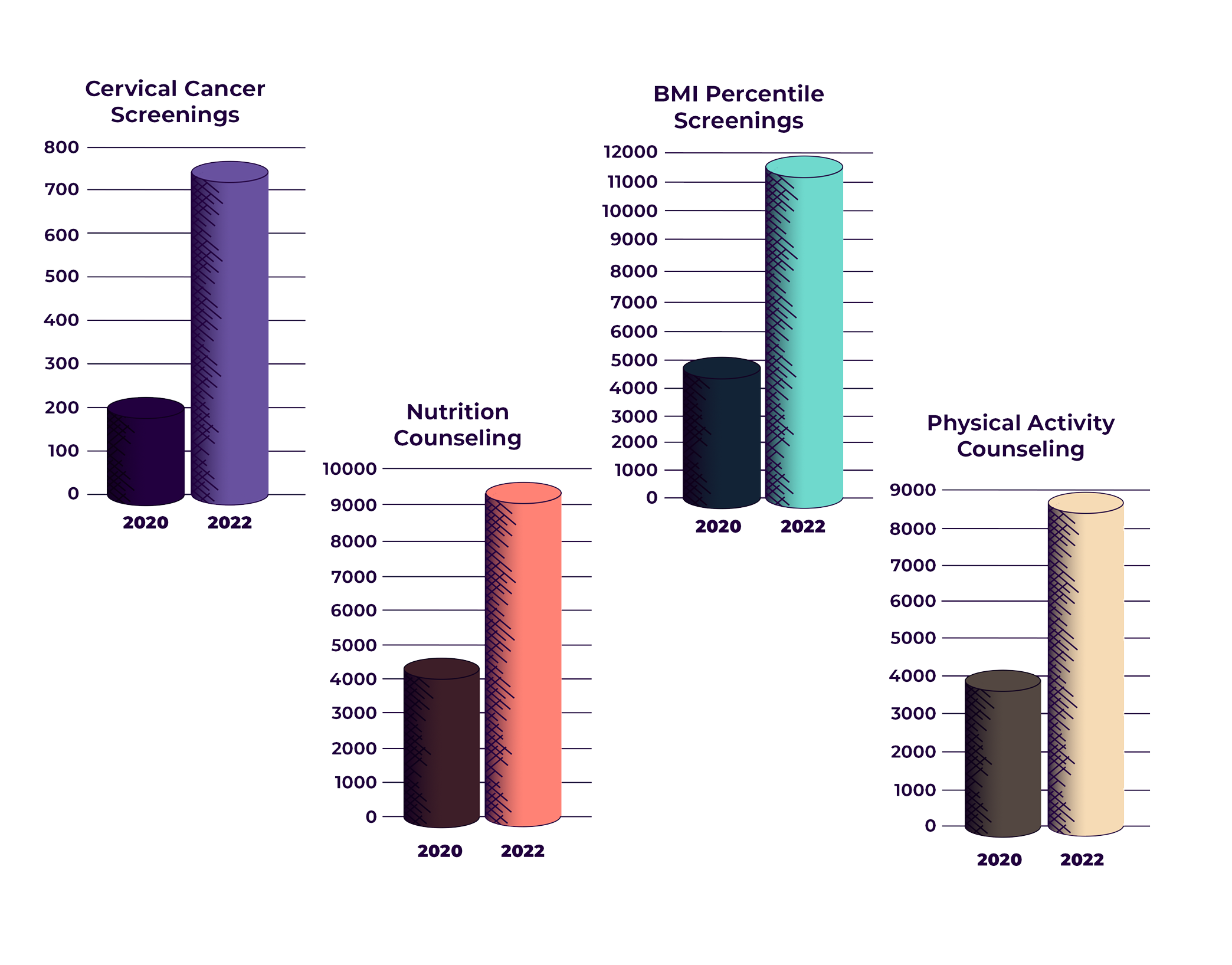
North Texas Quality Improvement Success
Another challenge at the start of Innovista’s partnership was that Medicaid providers were falling well below performance goals for various quality metrics.
Innovista worked with providers to improve these metrics by sharing regular performance reports that indicated areas for improvement, holding coaching sessions, implementing a health information exchange, and offering provider engagement incentives.
Within two years, medical loss ratio (MLR) dropped from 106% (indicating a big loss in revenue) to 76%. This resulted in a significant increase in shared savings—$38 million between 2020 and 2022.
Performance data for several quality metrics also increased significantly in two years:
Cervical cancer screenings: 754 completed in 2022 (+554 from 2020)
BMI percentile screenings: 11,702 completed in 2022 (+6,855 from 2020)
Nutrition counseling: 9,320 completed in 2022 (+4,970 from 2020)
Physical activity counseling: 8,797 completed in 2022 (+4,860 from 2020)
Partners
Innovista partnerships with community-based organizations provide CHWs with critical resources to address SDOH in a meaningful way. Partnerships include behavioral health resources, transportation and food insecurity services, on-demand mobile urgent care, and FindHelp.org, which helps CHWs locate free or reduced-cost resources in their area.

Behavioral health resources for patients in the comfort of their own home.

Enables patients, case managers, and community health workers to find free or reduced-cost community-based programs to address SDOH.

Behavioral health resources for patients in the comfort of their own home.